By Nadia Marshall
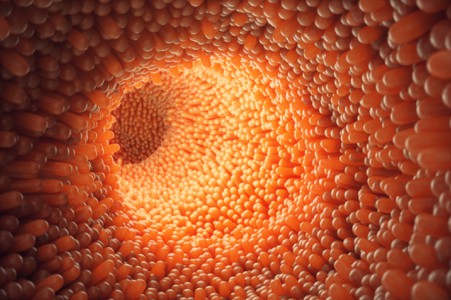
I'm about to take you on a (relatively short) journey into our large intestines (pictured above) and explore the weird and wonderful world of fibre and the microbiome...
...this will lead us to the immune system and how eating a predominantly plant-based diet with lots of fibre can directly affect our virus-fighting memory T-cells.
This is a tale of two fibres; insoluble and soluable.
Insoluable fibre is what we mostly imagine when hear the word 'fibre'. It is made up of cellulose and hemi-cellulose from carbohydrates (namely grains, legumes, spices, seeds, nuts, fruits and veggies) that resists digestion in the small intestine.
Most of this fibre contributes to 'fecal bulking' but some of it is deposited in the tiny crevasses of the gut, building little micro-environments for our gut bacteria to live in, referred to as 'food webs' (1).
Soluable fibre dissolves in water, forming a gel-like consistency (think dissolved psyllium or soaked chia seeds). It doesn't contribute to 'fecal bulking' but rather collects in the large intestine and is slowly fermented by gut bacteria. It is very sticky in consistency, like a gel.. so you can imagine it sticking to the collections of insoluable cellulose in the gut.
So our gut bacteria now has a lovely little house to live in made of stick-like cellulose stuck together with a lovely gel-like mortar. This house gives it protection but also food. The bacteria slowly digests both the sticks and the mortar (the soluable and insoluable fibre) through fermentation and turns them both into short-chain fatty acids (SCFA) (1).
Short-chain fatty acids are so called because they are fatty acids with less than six carbon atoms. They're so small, they can be easily absorbed through the gut wall. The three SCFAs produced through the fermentation of fibre are Acetate, Propionate and Butyrate.
You may have heard of these before. Acetic acid is naturally found in vinegar, especially Apple Cidar Vinegar; propionic acid is naturally found in milk, cheese and yoghurt; and butyric acid is naturally found in butter and ghee.
So we can think of our litte gut bacteria fermentation dens as teeny tiny vinegar, cheese and ghee making factories!
These SCFAs have a variety of incredible roles to play in the body. Butyrate is used as an energy source in the cells of the large intestine... like little colon power stations! When the colon cells use butyrate for power, they consume oxygen which contributes to a more oxygen-free or anaerobic environment in the gut. This in-turn supports the proliferation of more butyrate-producing bacteria. A positive feedback loop. So cool.
SCFAs are also absorbed into blood circulation via the portal vein and liver where they act as signaling molecules and help regulate a variety biological processes' (1). For example, acetate helps reduce inflammation and plays a role in the systemic correction of the blood (4); butyrate also reduces inflammation, helps with inflammatory bowel disorders and colitis and protects against colorectal cancer (3,4); while propionate is known to help us feel satiated after eating and reduce cholesterol levels (4).
Inside the intestine, the SCFA help to produce a lovely thick layer of mucous over the entire gut wall, protecting it from bacterial penetration, inflammation and damage from the bacterial fermentation process (which is acidic). Without this juicy wall of mucous we become suceptible to infections and chronic inflammatory diseases (1).
But what we specifically want to know about is the effect of SCFAs on our immune system. The main SCFA to consider here is butyrate or butyric acid and their effect on T-cells.
T-cells are white blood cells that are an essential part of our immune system. They either act as 'killer cells' whereby they recognise an antigen (a foreign substance) and kill it... or they act as 'helper cells', helping our B cells to create antibodies.
Butyrate has been shown to promote the long-term survival of activated T-cells as well as enhancing their memory potential (2). Activated T-cells (also known as 8+ T-cells) specifically attack virus-infected cells and tumours, including cancers. They also help to regulate or restrain certain types of immune responses, like a cytokine storm (5). So they're super important when it comes to COVID-19, including both vaccine-induced immunity and natural immunity.
So how do we particularly increase our bacterial production of butyrate? It has been shown that eating a type of fibre called Resistant Starch increases our production (4). Resistant starch is found in many foods but is especially high in oats, rice, potatoes, wheat, sweet potatoes, beans, legumes and green bananas. If you cook and then cool your grains, potatoes and pasta, the resistant starch levels are even higher. For example, we often cook rice for lunch then have the left over rice for dinner. We'll heat up our daal in the evening but not the rice... so it'll be high in resistant starch.
So there you have it. The connection between fibre, gut bacteria, SCFAs and T-cells. The moral of the story is... eating a predominantly plant-based Ayurvedic diet with plenty of oats, rice, legumes, pulses, spices, veggies, fruits, nuts and seeds is a wonderful thing for your gut health and immune strength. And, eating a generous amount of ghee with these foods will also help to increase your butyrate levels directly.
References
1) Science Direct: The Impact of Dietary Fiber on Gut Microbiota in Host Health and Disease (This is a brilliant article worth reading if feeling geeky)
2) PubMed: Microbiota-Derived Short-Chain Fatty Acids Promote the Memory Potential of Antigen-Activated CD8 + T Cells
3) ResearchGate: Immunology. Feed your Tregs more fiber
4) OxfordAcademic: Fecal Butyrate Levels Vary Widely among Individuals but Are Usually Increased by a Diet High in Resistant Starch
5) Nature Reviews Immunology: T Cells Calm the Storm
How Fibre Nourishes Long-term Immunity